I’ve had a cochlear implant since 2009. If you’ve read about my initial experience with the implant (in my book “Shouting Won’t Help” and elsewhere), forget everything I said (about cochlear implants… I stand by the rest of it). It’s a whole new world out there.
The October meeting of the New York City Chapter of the Hearing Loss Association of America made it clear how much things have changed. And all for the better.
Cochlear implants are increasingly popular, and not just because of our aging population. The eligibility requirements for a cochlear implant (which are set by Medicare) were broadened in 2022 after a study showed benefits in those with less severe loss than had previously been the cutoff. Medicare pays 80% of the cost of the device, with the other 20 percent covered by Medicaid or a Medigap program.
Even though I had virtually no hearing in my left ear for about two decades, I did not meet the then more restrictive criteria. The loss in my good ear was moderate to severe, partially corrected by a hearing aid. A prolonged period of deafness before a cochlear implant doesn’t bode well for success, although there are exceptions. These days even those with single-sided deafness qualify, thanks in part to advocacy by the American Cochlear Implant Alliance, which also has a good discussion of implants on their website.
Audiologists are usually the first to suggest a cochlear implant. If you’re interested, they will send you for an evaluation. If you qualify, the next step is to find a surgeon. It might be an ENT you already know, but more likely you’ll need someone at a major medical center with a strong cochlear-implant program. The surgery is easy for the patient but requires a highly skilled surgeon trained in the procedure.
Don’t get too hung up on the doctor, however, because except for checkups, an audiologist (one who specializes in cochlear implants) will be your guide for the months and years that follow. It is the audiologist who will activate your implant, a few weeks after surgery, and he or she will program and re-program the device as you adjust to it, optimizing your ability to “hear” via the digital signals.
How do you choose a brand? Three manufacturers have FDA approval to market cochlear implants in the U.S. These are Advanced Bionics, Cochlear Americas and MED-EL. Most experts say that all are good, leaving the decision to the patient. But there are objective reasons to choose one brand over another. If you prefer a single headpiece with no behind-the-ear component, for instance, you might choose Cochlear’s Kanso or the MED-EL Rondo You may be allergic to the metal in one brand, but not another. The behind-the-ear fit of one or another brand may work better for you.
Talk to people who have implants. Back in 2009, I knew no one with a cochlear implant and I had never heard of HLAA. Today, it’s easy to be connected to a network of cochlear implant recipients through HLAA or through the manufacturers. There is a lot of information online and in books. I’m just skimming the surface in this post.
The big difference today is what happens in the months immediately following activation of the implant. These days, auditory rehabilitation with a speech-language therapist is widely offered. In-person rehab can make a huge difference in speech comprehension. Cochlear-implant recipients need dedicated time to get used to the new way that sound is being transmitted to the brain, and auditory rehab can be enormously helpful with that.
Is it the right time for you to get an implant? This depends not only on the objective criteria measured by hearing tests, but also where you are in your life. When I got my cochlear implant, I was still working and in a very competitive workplace. I couldn’t afford to spend the early weeks and months using only the C.I. and not my hearing aid, as had been recommended. Audiologists today often encourage patients to return to work. Meghan Despotidis, an audiologist at Columbia University Medical Center, who moderated our chapter panel discussion, encourages newly implanted patients to return to work, with a hearing device in the other ear if needed. “If forces the CI to be immersed in speech,” she said, “which can help improve word understanding.”
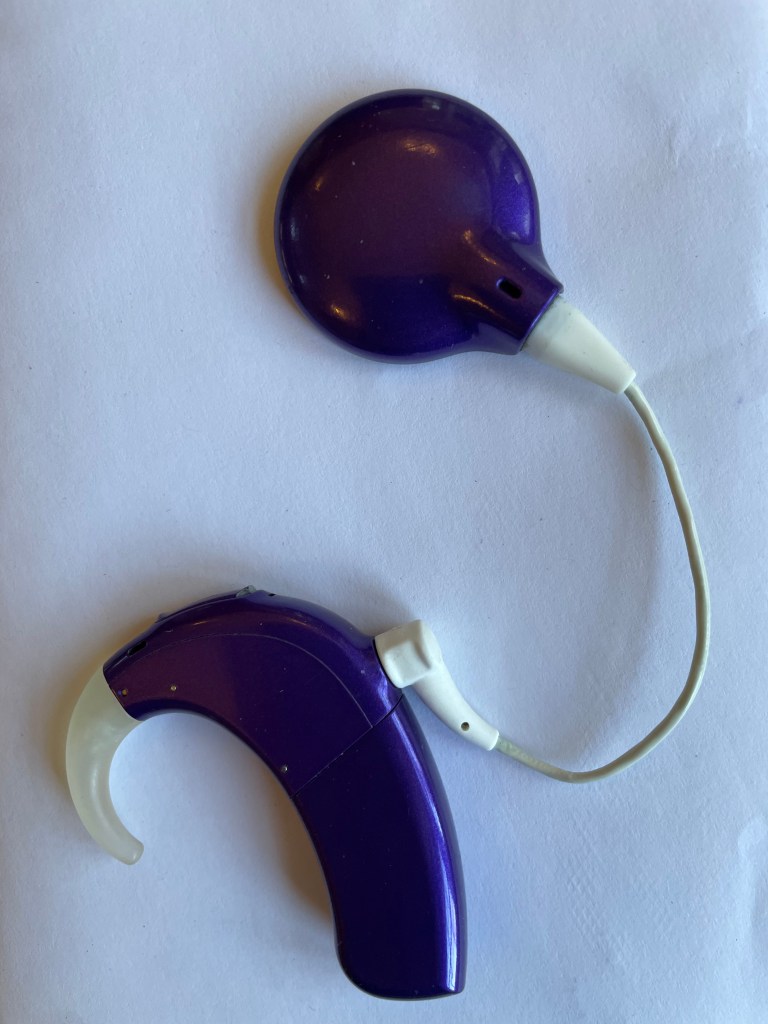
Should you wait for better technology? Most experts say the sooner you get the implant, the better the outcome. The internal implanted device that I got 14 years ago is very similar to those implanted today. One notable improvement is the ability to preserve residual hearing in the implanted ear, but I had almost no residual hearing, so didn’t miss much. There are occasional problems that require the implanted device to be replaced but in general it’s the external processor that is regularly updated. This is the earpiece, which connects via a small cable to the magnetized headpiece that connects to the implant itself. I have had two upgrades over the years and each time the new processors were more comfortable physically (a smaller behind the ear component) and provided improved speech perception.
Our chapter meeting focused on the experiences of two recent implant recipients – one was an adult who lost her hearing late in life. The other was a bilaterally implanted teenage boy who got his first implant at the age of one year. Both regarded their implants as something of a miracle, and their stories were deeply moving. The captioned video will be available at hearinglossnyc.org, in a week or two. Look under “Programs.”
I love my cochlear implant. It’s bright purple. See photo.
**
You can also read my books:


Another awesome update from Katherine!
LikeLike
Thank you!
LikeLike
Thank you
LikeLike
Thanks , Katherine! I too love my. implant. I was 86 when I was implanted four years ago . My brain thanks me every day for making it easier to hear. The implant lowers my fatigue level because my brain does not have to burn a lot of extra physical energy to understand conversations, a huge plus when you are 90.
LikeLike
I learn a lot from you about hearing implants etc.. I have new in the ear aids and I’m upset wit them( starkey) the voice is too loud and I have nothing to control this accept back to Doctors. At 90 years old it is difficult. I’m thinking return so I don’t loose my $3,000 dollars I must pay her $300.00 for the aids..
your very kind to share with us. Thankyou. Dorothy Carlson….
LikeLike
Hi Dorothy, Can you control the volume? You may just need to turn it down. Also, has the audiologist reprogrammed your hearing aids since you got them? It sounds as if they’re not set correctly for you. Hearing aids often have to be reprogrammed until you get the right mix of sounds.
Ask your audiologist if that could be done remotely — I know it’s possible but I don’t know if audiologists will do it.
Thank you for commenting, and I hope the hearing aids work out for you. Starkey is a good brand.
LikeLike
Shouting Won’t Help was my first introduction to understanding my hearing loss, and “Forget everything I just said” is undoubtedly a huge exaggeration. That book helped me go quickly from a complete ignoramus to a member of HLAA and gradually to someone who could help others. Two sets of hearing aids later, my hearing loss was so severe that I, too, received a pair of cochlear implants. And they were a game-changer for me, too. But the essential messages in your books about compensatory practices, technologies, etc., remain. I owe you, HLAA, my CI surgeon, my audiologist, and others for the help that returned me to life.
LikeLike
What a wonderful, generous comment.
Thank you!
I didn’t mean to suggest readers forget everything I said in the book, just my initial negative experience with the cochlear implant.
LikeLike
Thanks for sharing this with us. I may need an implant in the future but want to be informed about what to expect. 🙌
LikeLike